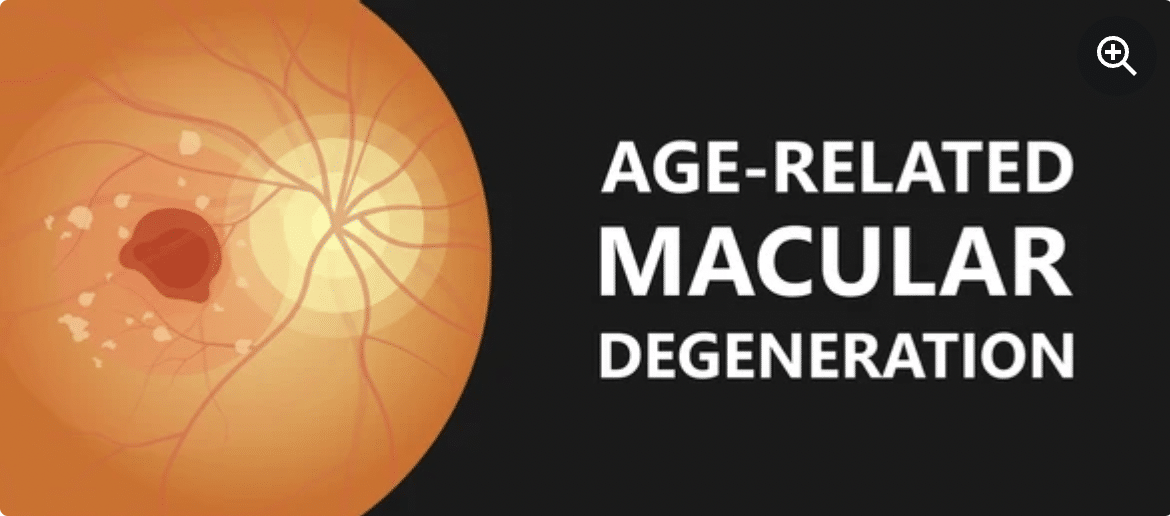
Macular Degeneration Treatment
Age Macular Degeneration (AMD) Treatment
What is macular degeneration?
Wet macular degeneration does not affect peripheral vision but can cause significant central vision loss.
Age-related Macular Degeneration (AMD) is a chronic eye disease that affects the part of the retina responsible for your central vision (the macula). The disease is one of the most common causes of vision loss in older adults. The disease typically causes “blurry” or “distorted” vision or a blind spot in the center of your visual field. It does not affect your side (peripheral) vision.
Age Macular Degeneration is one of the two types of disease. The other type – dry macular degeneration – is more common and less severe. Affecting only 10 to 15 percent of those with macular degeneration, the wet type always starts out as the dry type.
Wet macular degeneration vision loss can be caused by:
Abnormal blood vessel growth. Sometimes abnormal new blood vessels grow under and into the macula. Also, these blood vessels can leak fluid or blood, interfering with the function of the retina.
Fluid buildup behind the eye, when fluid seeps under the retina. Also, it can build up and cause a lump in the macula.
Especially, if you notice any changes in your vision, see an eye doctor regularly and as soon as possible. Also wet AMD can occur suddenly and progress rapidly. Therefore, treatment can help slow vision loss and maintain independence.
Symptoms of the Disease
Wet AMD symptoms often appear suddenly and worsen rapidly. These may include:
- Visual distortions, such as straight lines that appear bent.
- Decreased central vision in one or both eyes.
- Need for brighter light when shooting close up or reading.
- Increased difficulty adapting to low light levels, such as when entering a dimly lit restaurant
- Increased blurriness of printed words.
- Decreased intensity or brightness of colors.
- Difficulty recognizing faces.
- A well-defined blurry spot or blind spot in your field of vision
The disease does not affect side (peripheral) vision, so it rarely causes complete blindness.
When to see a doctor
See your eye doctor if:
- You notice changes in your central vision.
- Your ability to see colors and fine details is impaired.
Especially, these changes may be the first sign of disease, if you’re older than 60.
Causes of the Disease
Although the exact cause of wet macular degeneration is unknown, it develops in people with dry macular degeneration. Particularly, about 20% of all people with AMD have the wet form.
Wet macular degeneration can develop in different ways:
Especially, vision loss caused by abnormal blood vessel growth. Sometimes abnormal new blood vessels grow from the choroid into the macula (choroidal neovascularization). The choroid is the layer of blood vessels between the retina and the outer, hard layer (sclera) of the eye. Also, these abnormal blood vessels can leak fluid or blood, interfering with the function of the retina.
Therefore, loss of vision cause by fluid accumulation at the back of the eye. When fluid leaks from the choroid, it can accumulate between the thin layer of cells call the retinal pigment epithelium and the retina, or within the retinal layers. Also, this can cause a lump in the macula, resulting in vision loss or deterioration.
Risk factors
Factors that can increase your risk of macular degeneration include:
- Age. This disease is most common in people over the age of 55.
- There is a family history and genetically inherited component of this disease. Researchers have identified several genes involved in improving the condition.
- Smoking or regular exposure to smoke significantly increases your risk of macular degeneration.
- Research shows that being obese increases the chance of early or moderate macular degeneration progressing to a more severe form of the disease.
- Cardiovascular disease. If you have diseases that affect your heart and blood vessels, your risk of macular degeneration may be higher.
Complications of the disease
Especially, people whose wet macular degeneration progresses to central vision loss are at higher risk of depression and social isolation. Therefore, with profound vision loss, people may experience visual hallucinations (Charles Bonnet syndrome).
Disease prevention
Particularly, it is important to have routine eye exams to identify early signs of disease. Also, the following measures can help reduce your risk of developing wet macular degeneration:
- Manage your other medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions to control the condition.
- Do not smoke. Smokers are more likely to develop macular degeneration than nonsmokers. Ask your doctor for help to quit smoking.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Choose a diet rich in fruits and vegetables. Choose a healthy diet filled with a variety of fruits and vegetables. These foods contain antioxidant vitamins that reduce your risk of developing macular degeneration. Add fish to your diet. Omega-3 fatty acids found in fish can reduce the risk of macular degeneration. Nuts like walnuts also contain omega-3 fatty acids.
Diagnosis of the Disease
Especially, your doctor will review your medical and family history and perform a complete eye exam. To confirm the diagnosis of macular degeneration, Your doctor may perform several other tests, including:
- Examination of the back of the eye. Your ophthalmologist will put drops in your eyes to widen your eyes and use a special instrument to examine the back of your eye. It will look for fluid or blood or a mottled appearance caused by drusen. People with macular degeneration often have multiple drusen – yellow deposits that form under the retina.
- Test for flaws in the center of your vision. During an eye exam, your eye doctor may use an Amsler chart to test for defects in your central vision. If you have macular degeneration, some straight lines on the chart will appear pale, broken, or distorted.
- Fluorescein angiography. During this test, your doctor injects a colored dye into a vein in your arm. The dye travels to the blood vessels in your eyes and highlights them. A special camera takes pictures as the dye travels through the blood vessels. The images will show if you have abnormal blood vessels leaking or retinal changes.
- Indocyanine green angiography. Like fluorescein angiography, this test uses an injected dye. It can be used to confirm fluorescein angiography findings or to identify abnormal blood vessels deeper in the retina.
Optical coherence tomography
This noninvasive imaging test shows detail sections of the retina. It describes areas of thinning, thickening or swelling. This test is also use to help monitor how the retina responds to macular degeneration treatments.
Optical coherence tomography (OCT) angiography. This is a newer, noninvasive test that, in some cases, allows your doctor to visualize unwanted blood vessels in the macula.
Dry macular degeneration Disease overview
Dry macular degeneration (DMD) is a common eye disease in people over the age of 50. It causes blurring or reduction in central vision due to thinning of the macula. The macula is the part of the retina responsible for clear vision in your direct line of sight.
The disease may first develop in one or both eyes and then affect both eyes. Over time, your vision can worsen and affect your ability to do things like read, drive, and recognize faces. But that doesn’t mean you’ll lose all your sight. Vision loss is typically central and people retain their peripheral vision. Some people have only mild central vision loss, while others may have it more severe.
Early diagnosis and self-care measures can delay vision loss due to DMD.
Symptoms of the Disease
DMD symptoms usually develop slowly and painlessly. These may include:
- Visual distortions, such as straight lines that appear bent.
- Decreased central vision in one or both eyes.
- Need for brighter light when shooting close up or reading.
- Increased difficulty adapting to low light levels, such as when entering a dimly lit restaurant.
- Increased blurriness of printed words.
- Decreased intensity or brightness of colors.
- Difficulty recognizing faces.
- A well-defined blurry spot or blind spot in your field of vision.
Generally, the disease can affect one or both eyes. If only one eye is affected, you may not notice any change in your vision, as your good eye can compensate for the weaker eye. And the condition does not affect side (peripheral) vision, so it rarely causes complete blindness.
DMD is one of the two types of age-related macular degeneration. It can progress to wet (neovascular) macular degeneration, which is characterize by growing and leaking blood vessels under the retina. The dry type is more common, but usually progresses slowly (over years). The wet type is more likely to cause a relatively sudden change in vision and cause severe vision loss.
When to see a doctor
See your eye doctor if:
- You notice changes in your central vision.
- Your ability to see colors and fine details is impaired.
Especially, these changes may be the first sign of macular degeneration, if you’re over 60.
Causes of the DMD disease
Especially, No one knows exactly what causes DMD. However, research shows it can be affected by a combination of heredity and environmental factors, such as smoking, obesity, and diet.
The condition develops as the tears age. Particularly, DMD affects the macula, which is the area of the retina responsible for clear vision directly in your line of sight. Over time, the tissue in your macula can thin and lose cells responsible for vision.
Risk factors
Factors that can increase your risk of macular degeneration include:
- This disease is most common in people over the age of 60.
- Family history and genetics. This disease has a hereditary component. Researchers have identified several genes involved in developing the condition.
- To smoke. Smoking or regular exposure to smoke significantly increases your risk of macular degeneration.
- Research shows that being obese can increase your odds of progressing to the more severe form of the disease from early or moderate macular degeneration.
- cardiovascular disease. Especially, ff you have diseases that affect your heart and blood vessels, your risk of macular degeneration may be higher.
Complications of the disease
People whose DMD progresses to central vision loss are at higher risk of depression and social isolation. With profound vision loss, people may experience visual hallucinations (Charles Bonnet syndrome). And dry macular degeneration can progress to wet macular degeneration, which can cause rapid vision loss if left untreated.
Disease prevention
It is important to have routine eye exams to identify early signs of macular degeneration. The following measures can help reduce your risk of developing DMD:
- Manage your other medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions to control the condition.
- Do not smoke. Smokers are more likely to develop disease than nonsmokers. Ask your doctor for help to quit smoking.
- Especially, maintain a healthy weight and exercise regularly. Also, If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Choose a diet rich in fruits and vegetables. Particularly, choose a healthy diet filled with a variety of fruits and vegetables. Also, these foods contain antioxidant vitamins that reduce your risk of developing macular degeneration.
- Add fish to your diet. Omega-3 fatty acids found in fish can reduce the risk of macular degeneration. Nuts like walnuts also contain omega-3 fatty acids.
Diagnosis of the Disease
Especially, your doctor can diagnose your condition by reviewing your medical and family history and performing a complete eye exam. Also, your doctor will do a few other tests, including:
- Examination of the back of the eye. Your ophthalmologist will put drops in your eyes to widen your eyes and use a special instrument to examine the back of your eye. It will look for a mottled appearance caused by drusen-yellow deposits that form under the retina. People with macular degeneration often have multiple drusen.
- Test for flaws in the center of your vision. During an eye exam, your eye doctor may use an Amsler grid to test for defects in the center of your vision. Macular degeneration can cause some straight lines in the grid to appear pale, broken, or distorted.
- Fluorescein angiography. During this test, your doctor injects a colored dye into a vein in your arm. The dye travels to the blood vessels in your eyes and highlights them. A special camera takes several pictures as the dye travels through the blood vessels. The images will show if you have retinal changes or abnormal blood vessels, which are a sign of wet macular degeneration.
- Indocyanine green angiography. Like fluorescein angiography, this test uses an injected dye. It can be used in conjunction with a fluorescein angiogram to identify specific types of disease.
Optical coherence tomography (OCT):
This noninvasive imaging test shows detailed cross-sectional images of the retina. Also, It identifies areas of retinal thinning, thickening, or swelling. Therefore, these can be cause by a buildup of fluid from blood vessels leaking into and under your retina.
Useful Links
About Eye Uveal Melanoma – Eye Cancer Treatment. Vitrectomy Retina Surgeries, About Keratoplasty Surgery. Strabismus Crossed Eye Squint Treatments, Diabetic Retinopathy Disease. Glaucoma Disease and Treatments. Retinitis Pigmentosa Disease and Treatments. Dry Eye Syndrome Treatments. Periodic Eye Examinations. What Is Macular Degeneration?(AAO Definition).
Your Expert Eye Surgeons

Education Information:
He completed his primary, secondary and high school education in Ankara. Fevzi Senturk graduated from Ankara University Faculty of Medicine with a degree in 1994, and subsequently received his Ophthalmology Specialization training from Eskisehir Osmangazi University Faculty of Medicine in 2000. Afterwards, Fevzi Senturk completed his Retina Fellowship at Istanbul Retina Institute and earned the title of Associate Professor at this institution. He is still continuing his academic career by taking the title of Professor at Istanbul Medipol University. He has focused his scientific and clinical studies on retinal diseases, Vitreoretinal surgery and cataract surgery.Awards,Memberships and Scientific Research:
- Retinal capillary hemangioma: AB interno surgical excision, 43rd National Congress Awards, Best Video First Prize, 2009
- Photodynamic therapy guided by indocyanine green angiography in chronic central serous chorioretinopathy, Turkish Journal of Ophthalmology, Best Publication Third Prize, 2000
- Retinal capillary hemangioma: AB interno surgical excision, 43rd National Congress Awards, Best Video First Prize, 2009
- Photodynamic therapy guided by indocyanine green angiography in chronic central serous chorioretinopathy, Turkish Journal of Ophthalmology, Best Publication Third Prize, 2000
- Vitreoretinal Surgery Techniques, Second Edition, Hayat Medicine Bookstore, 2008
- Eye Diseases and Anti-VEGF Therapy 2010.
- Ocular Electrophysiology (TOD Education Publications No 13) Meaning of VEP, VEP registration and parameters in ISCEV standards., 2011
- Clinical Eye Atlas (Oxford Atlases in Ophthalmology), 2012
- Imaging in Ophthalmology, Microperimetry, 2013
- Ocular Electrophysiology (TOD Education Publications 1st Edition), Multifocal Electroretinogram Recording and Evaluation, 2022.
- Current Vitreoretinal Surgery (TOD Education Publications), Surgical Anatomy of the Retinal and Vitreous, 2022.
- Turkish Medical Association
- Turkish Ophthalmology Association
- Turkic Republics Ophthalmology Association
- Electrodiagnostic unit board membership
- Electrodiagnostic unit training representative
- International Society for Clinical Electrophysiology of Vision (ISCEV)
Specialized Treatments and Surgeries:
- Macular Degeneration Disease and Treatments
- Retinal Detachment Treatments
- Retinal Hemorrhages Due to Diabetes and Hypertension and Their Treatments
- Retinitis Pigmentosa Treatments
- Central Serous Chorioretinopathy
- Retinal Vascular Occlusions
- Epirentinal Membrane
- Macular Hole
- Glaucoma eye pressure
- Neuroophthalmological Diseases
- Vitrectomy-Retina Surgery
- Intravitreal Injection Treatments
- Argon Laser Photocoagulation Treatment
- Photodynamic Therapies
Foreign language:
- English
MEDICAL UNIVERSITY of Ankara
28 Years of Experience
>25.000 Surgery
Definitely avoid low-cost Eye Treatment
You may think that a cheap eye treatments is right for you. This might be fine if you're buying a cheap TV, but it's not worth the gamble with your eyesight. But as you know, having cheap eye surgery means sacrificing technology, physician quality, medical care and sterile conditions, and most importantly, taking risks. The issues that fall on a patient who wants to have cataract surgery and should pay the most attention; The hospital with the latest technology in cataract surgery and imaging devices, a sterile environment, and an experienced doctor and clinical team should be selected. We would like to remind all our patients that they only have two eyes and that the most important and most sensitive sense organ is their eyes.
None of these things are more important than your eye health, and we do not compromise on quality and cutting-edge technology. We offer you our prices in a very understandable, fair and affordable way.
There are no hidden costs in our pricing. We make eye treatments affordable for you.